Bringing Urgent Care to Rural Zimbabwe: How Solar-Powered Mobile Health Clinics Are Transforming Access

In Zimbabwe, more than 60% of the population resides in rural regions where healthcare access is hindered by long distances, high costs, and inadequate infrastructure. Many individuals trek 15 to 20 kilometers to reach the closest health facility, often postponing medical attention until conditions worsen significantly.
Chiedza Mushawedu, the co-founder and executive director of ZimbosAbantu Healthcare on Wheels, encountered these obstacles firsthand during her tenure at a private hospital in 2016. She recalls, “We witnessed preventable fatalities from curable illnesses, unattended home births without professional care, and numerous undiagnosed chronic diseases simply because healthcare was inaccessible.”
In response, Chiedza launched ZimbosAbantu in 2021 with the mission to bridge healthcare gaps in underserved communities. The initiative transforms vans into solar-powered, technology-equipped mobile clinics, delivering medical services directly to remote populations. This innovation has reduced the average travel distance from 15 kilometers to just three, enabling timely diagnosis and treatment within local neighborhoods.

Healthcare Delivered on the Move
Currently, ZimbosAbantu operates a fleet of ten mobile clinics, each carefully positioned to serve the most vulnerable communities. According to Chiedza, these clinics are fully outfitted to function independently in off-grid locations. Solar panels with battery storage power the units, which include refrigeration systems for vaccines and medications, alongside a compact diagnostic laboratory featuring the HealthCube device. This portable lab conducts over a dozen critical tests such as blood sugar, hemoglobin levels, and malaria detection.
Launching each mobile clinic demands a blend of financial investment, infrastructure, and skilled personnel, with setup costs around US$120,000 per unit. The clinics offer a broad spectrum of services including primary care, maternal and child health, dental and vision care, immunizations, HIV testing, and screenings for non-communicable diseases (NCDs) like hypertension and diabetes. “We focused on delivering essential, cost-effective services that address the most pressing health concerns in these areas,” Chiedza notes. Complex cases are referred to partner hospitals under the oversight of the Ministry of Health and Child Care.
Enhancing the Patient Journey
Community health mobilizers act as the first point of contact, providing health education and conducting preliminary blood pressure screenings. Upon arrival at the mobile clinic, patients are digitally registered. “For many, this is their first experience with a digital health record,” Chiedza explains. This system enables continuous monitoring of chronic conditions such as diabetes and hypertension, even as the clinic relocates.
Patients then proceed to triage for vital sign assessments before consulting with a nurse or doctor who evaluates their condition and provides a diagnosis. If medication is necessary, it is dispensed immediately from the solar-powered pharmacy fridge. Follow-up appointments are scheduled for subsequent visits as needed.
The vans are thoughtfully designed to be accessible, featuring ramps for individuals with disabilities, private consultation rooms, and staff trained in gender-sensitive care.
On average, each mobile clinic attends to 18 to 25 patients daily, balancing quality care with broad reach. “Our ambition is to ensure healthcare is available within one kilometer of every household in the communities we serve,” Chiedza emphasizes.
Beyond patient volume, ZimbosAbantu employs a comprehensive data system tracking 18 key health indicators on daily, weekly, monthly, and annual bases. These metrics cover the entire spectrum of HIV and NCD care, from prevention and screening to chronic disease management and palliative services.
“We focus on outcomes, not just numbers,” Chiedza states. “Our data reveals trends in maternal health, vaccination rates, chronic disease control, and shifts in sexual and reproductive health behaviors.”
The organization monitors patient visits, maternal health consultations, immunizations, NCD screenings, HIV testing, and follow-up care, using this information to refine services. They also contribute data to the national health database, supporting government health planning and advocacy. “Since 2021, our evidence has demonstrated tangible impact,” she adds, highlighting collaborations with local and international health partners attracted by their success.
To enhance clinical decision-making, ZimbosAbantu collaborates with Econet Wireless to enable telemedicine connectivity. This allows nurses to consult with remote physicians instantly, improving diagnostic accuracy and expanding access to expert care. “Technology links rural clinics with urban doctors, enabling faster, more precise treatment,” Chiedza explains.
In areas with limited internet access, real-time data collection is challenging. ZimbosAbantu addresses this by using solar-powered equipment, offline-first health software, and encrypted cloud storage to safeguard patient data. Portable devices like ultrasounds and glucometers synchronize automatically once connectivity is restored.
A Community-Driven, Tech-Enabled Funding Approach
In addition to mobile healthcare delivery, ZimbosAbantu confronts financial barriers through its Chikwama Mukando weHwutano initiative, a community health savings scheme inspired by Zimbabwe’s traditional mukando (rotational savings group). Families contribute as little as US$3 monthly to access subsidized healthcare services.
“Small monthly contributions from families provide subsidized consultations, screenings, and discounted medications, distributing costs across the community,” Chiedza explains. Nearly 1,000 members currently participate. The fund also offers microloans to women-led enterprises, linking health access with economic empowerment. Digital tracking, flexible payment plans, and community education minimize defaults and encourage sustained involvement.
“Operating a single mobile clinic costs about US$5,000 monthly,” she notes. “Serving an average of 16 patients daily helps us break even, while Mukando weHwutano keeps care affordable for users.” This integrated model combines healthcare financing with community economics, ensuring no one is denied care due to financial constraints and fostering local ownership. “It’s a fusion of health and empowerment,” Chiedza adds.
Overcoming Obstacles and Expanding Reach
Rolling out mobile clinics nationwide has presented several challenges. Initially, regulatory hurdles around licensing and official recognition of mobile clinics as legitimate health facilities slowed progress. “We had to demonstrate that mobile clinics could uphold the same standards as fixed facilities,” Chiedza recalls. “Once proven, the Ministry of Health and local authorities supported our efforts.”
ZimbosAbantu now operates under formal agreements with the Ministry of Health and Child Care, the National AIDS Council, and local governments. Each mobile unit is linked to a hospital or clinic for patient referrals and medical waste management. Their work aligns with Zimbabwe’s Vision 2030 objective, which aims to ensure no citizen must travel more than 10 kilometers to access healthcare-a goal still unmet in many rural areas.
Building trust within communities was another significant hurdle. “We engage local leaders, conduct free health outreach campaigns, and demonstrate consistent impact to earn trust through visibility and reliability,” Chiedza explains.
Financial sustainability remains a critical concern. Initially funded with US$22,000 from personal savings, ZimbosAbantu is now seeking to raise US$6 million over the next three to five years through a blended financing strategy. This capital will support the deployment of 50 new mobile clinics across all ten provinces, procurement of medical equipment, and operational expenses.
As a woman leading a healthcare innovation in a male-dominated sector, Chiedza faces gender-specific challenges. With nearly 20 years of experience, including international roles at the Dubai World Trade Centre and Zimbabwe’s private healthcare sector, she acknowledges, “Gender bias and limited funding access are ongoing obstacles. However, mentorship programs like Impact Hub, AWEC, AWE, and the Nkwanzi Fellowship have been invaluable. Persistence and collaboration fuel my journey.”
The greatest current challenge is scaling rapidly enough to meet increasing demand. “Communities are requesting more specialized services and broader coverage, but funding and skilled personnel remain limited. We are actively pursuing partnerships and investments to close this gap,” she says.
Future Prospects
Since its inception, ZimbosAbantu has served over 138,000 patients, reached 15 underserved communities, created more than 48 full-time jobs, and trained upwards of 100 community health mobilizers.
In 2025, the organization earned the prestigious Bayer Foundation Women Empowerment Award, recognizing its innovative impact. “This honor is a tribute not only to my work but to the communities we serve and the dedicated team behind ZimbosAbantu Healthcare on Wheels,” Chiedza reflects.
Looking forward, the team plans to expand the number and reach of mobile clinics, develop specialized units for maternity, dental, and eye care, and integrate AI-powered diagnostics, wearable health monitors, and teleconsultation hubs to enhance data-driven healthcare delivery.
“Our vision is to establish ZimbosAbantu as a regional pioneer in mobile, technology-driven primary healthcare, demonstrating that innovation and equitable access can coexist,” Chiedza concludes.
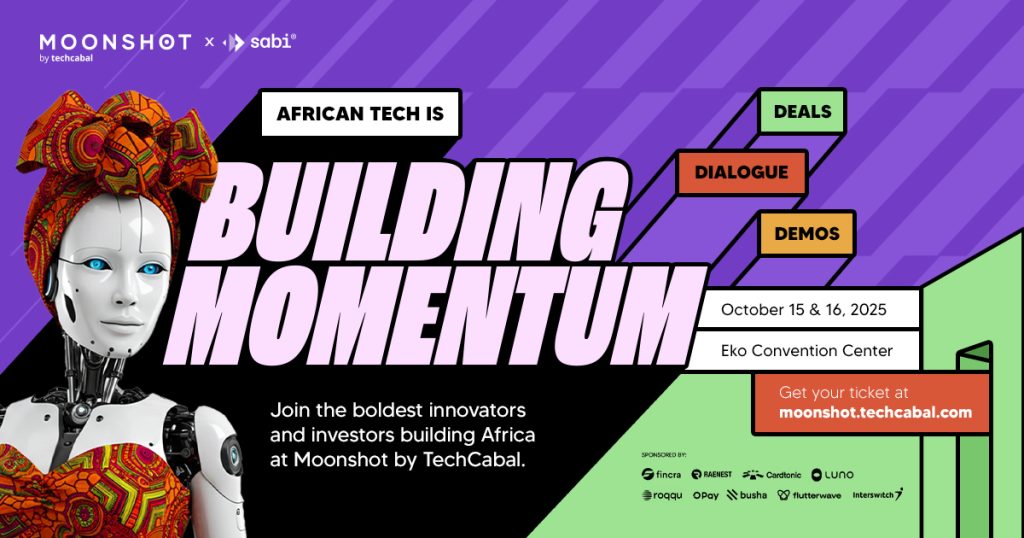
Save the date! Moonshot by TechCabal returns to Lagos on October 15-16! Join Africa’s leading founders, creatives, and tech innovators for two days of inspiring keynotes, networking, and forward-thinking ideas. Secure your tickets now at moonshot.techcabal.com






Leave a Reply